Endometrial cancer is the most common malignant tumour after breast cancer.
Led by Dr Juan Mario Troyano Luque, Professor of Obstetrics and Gynecology and President of the Governing Council and Advisor of the Spanish Society of Gynecology and Obstetrics (SEGO), we analyse what endometrial cancer is, its causes and symptoms, as well as its treatment and possible complications.
What is the endometrium?
The endometrium is the tissue that lines the inside of the uterine cavity. It comprises large glands, arteries and veins and is expelled outside the uterus in the form of monthly menstrual bleeding, generally every 28 days. For this reason, the endometrium is subject to great dynamism each month, where three well-defined stages concur in evolution:
Development phase: is the first stage of growth after menstruation, produced by the action of estrogens, acquiring its largest size 14 days after the period.
Stabilisation Phase: lasts about ten days and corresponds to the period of greatest glandular and vascular volume due to the action of progesterone, this being the phase where the beginning of pregnancy is favoured.
Desquamation or menstruation phase: will occur, as long as a pregnancy does not happen, due to the marked decrease in both hormones (estrogens and progesterone).
This changing dynamism of the endometrium in women with periods is a fact that preserves it from possible cancer. On the contrary, in those women in whom these changes do not occur or do not have menstruation, the risk of suffering from this cancer is more significant.
What is endometrial cancer?
Endometrial cancer is the most common gynaecological malignancy after breast cancer and occurs in the tissue that lines the walls of the uterus, called the endometrium. It is probably, if it is diagnosed and treated in time, cancer that produces less severity and less mortality in the woman who suffers from it.
Who does it affect?
80% of endometrial cancer occurs in postmenopausal women without periods. The age of onset is calculated, on average, from 10 years after menopause, that is, approximately 60 years. However, 20% occurs in menstruating women and 5% in women under 40.
What are your causes?
Malignant tumours of the endometrium are related to the action of estrogen for a long time since it is the hormone that stimulates their growth, causing a sustained increase in the volume of the endometrial glands (hyperplasia). This is the most frequent cause of the appearance of this cancer and also the one with the best prognosis since it produces a glandular proliferation very similar to normal glands and cells.
Even so, it must be considered that, regardless of this possible cause, not all women undergoing hormonal treatment develop endometrial cancer since there must be a predisposition for this malignant lesion to occur.
This type of cancer usually occurs in women with less menopause time (the first five years after the withdrawal of the rule). In addition, it usually has a prolonged evolution. It passes, before being cancer, by a benign glandular overgrowth called simple epithelial hyperplasia and, later, by a premalignant atypical glandular hyperplasia.
The remaining 30% of these cancers are not related to hormones and occur in patients who have obvious signs of genital atrophy, with poor cell growth, but with the presence of abnormal cells. For this reason, they have the worst prognosis as they present autonomous development, independent of hormones. This form of endometrial cancer usually occurs in older women.
Other factors that influence the appearance of endometrial cancer are:
- Estrogen treatments for a long time without associating them with progesterone, especially in women with hormonal therapy in menopause.
- Obesity, since fats trigger the production of a hormone, estrone, similar to estrogen.
- Diabetes, associated with obesity, is common in this disease.
What are the symptoms of endometrial cancer?
The most frequent sign of suspicion of endometrial cancer is the appearance of genital bleeding after menopause in women who have not had periods for years. Although this is the most promising sign, it should be noted that only 3% of menopausal women with genital bleeding have endometrial cancer since the remaining 97% are due to other causes that are not necessarily cancerous.
The discharge of pus from the genitals at ancient ages can also be a sign of suspicion, caused by a narrowing of the canal of the cervix, which promotes the accumulation of necrotic cellular material within it.
Complications of endometrial cancer depend on the degree of severity and extent of the tumour.
Younger menstruating women may also be at risk for endometrial cancer, although with a lower incidence. In them, other less striking signs that the gynaecologist must always take into account during the examination are:
- Women with abnormal genital bleeding outside the rule (metrorrhagia).
- Women who do not ovulate (anovulatory cycles).
- Women who have a sudden and abundant change in their periods (menorrhagia).
- Obese women, above all, are morbidly obese and also have a family history of breast or endometrial cancer.
- Young menopausal women below 40-45 years.
- Women with polymicrocystic ovaries due to not have periods for long periods.
- Women were treated with estrogens for a long time without associating progesterone.
Although it is considered debatable, women were operated on for breast cancer and treated with Tamoxifen, a class of drugs known as antiestrogens, for periods of more than five years.
What is the treatment for endometrial cancer?
The most advisable thing is to treat the hyperplasia, that is, to diagnose early the increase in the abnormal development of the endometrium and to identify risk factors such as obesity, diabetes and a family history of breast and endometrial cancer.
Preventive treatment is aimed at associating progesterone when it is necessary to treat women with estrogen for a long time. When in doubt, the specialist will safely perform an endometrium biopsy to check its histological status.
Since contraceptives associate both hormones, it is an excellent option for reducing endometrial thickness. In principle, these tend to preserve the appearance of endometrial cancer in women who have previously taken them.
About endometrial hyperplasia, if it is simple or complex but without atypia (changes in cell morphology) and in young premenopausal women who have not had children, treatment with progesterone can be considered to cause a decrease in endometrial thickness. In addition, a control biopsy will be performed to verify said regression.
If, after approximately one year, the endometrial volume has not returned to regular, simple removal of the uterus should be considered.
In general, the best treatment for endometrial cancer is the initial diagnosis, based on:
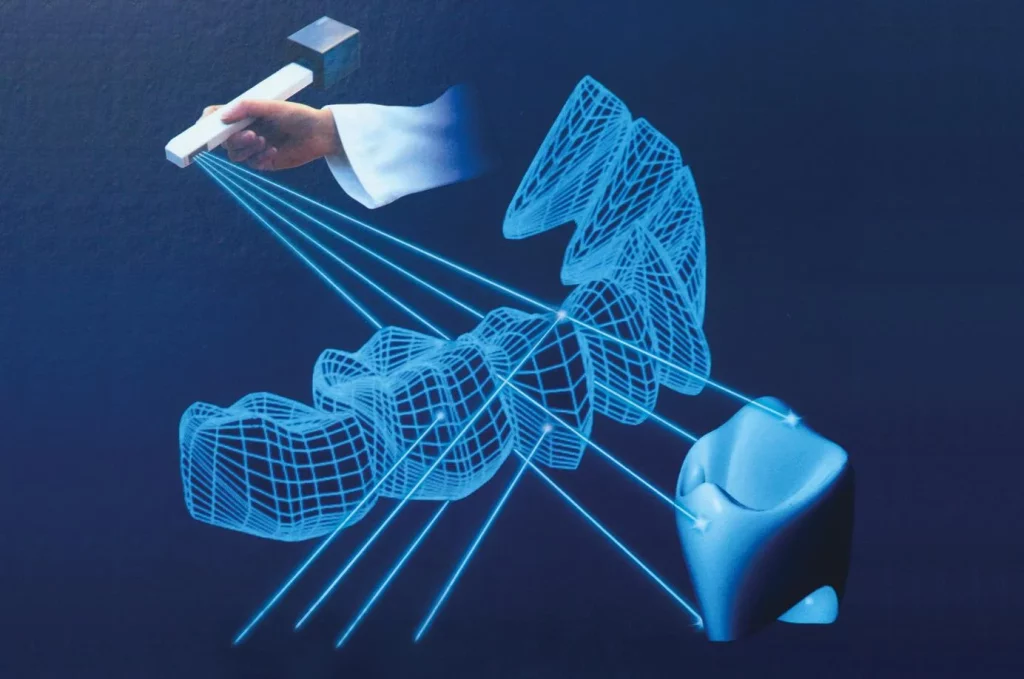
Transvaginal ultrasound: allows you to see very thickened and irregular endometrium with many arteries, what proportion of invasion exists in the uterine muscle and if it extends to the cervix.
Endometrial cytology: obtaining a sample of the endometrium for analysis.
Hysteroscopy: A procedure to examine the inside of the uterus.
Nuclear Magnetic Resonance (NMR): assesses the infiltration of the uterine muscle and if there is an extension to other pelvic organs.
State-of-the-art Computerized Tomography (CAT): assesses lymph node involvement and the distance extension of the tumour.
Surgical treatment and operative complexity in endometrial cancer will depend on tumour invasion.
Laparoscopic or robotic surgery: today, this surgery minimises the sequelae derived from the operative act.
In cases of advanced disease with lymph node involvement, oncological treatments with chemotherapy and radiotherapy will be necessary to improve survival and are always under the control of oncology specialists.
What complications do you have?
Complications of endometrial cancer depend on the degree of severity and extent of the tumour.
Atypical hyperplasias and non-invasive tumours only require simple removal of the uterus, with an excellent prognosis. Invasive endometrial cancers, depending on the degree of invasion, will require more complex surgery and chemotherapy and radiotherapy treatments. Complications will depend on the aggressiveness of these treatments, always in the hands of accredited specialists in this field.